Opinion
Panorama: Osteoarthritis and the Role of Physiotherapy
Published
2 years agoon
By
Eric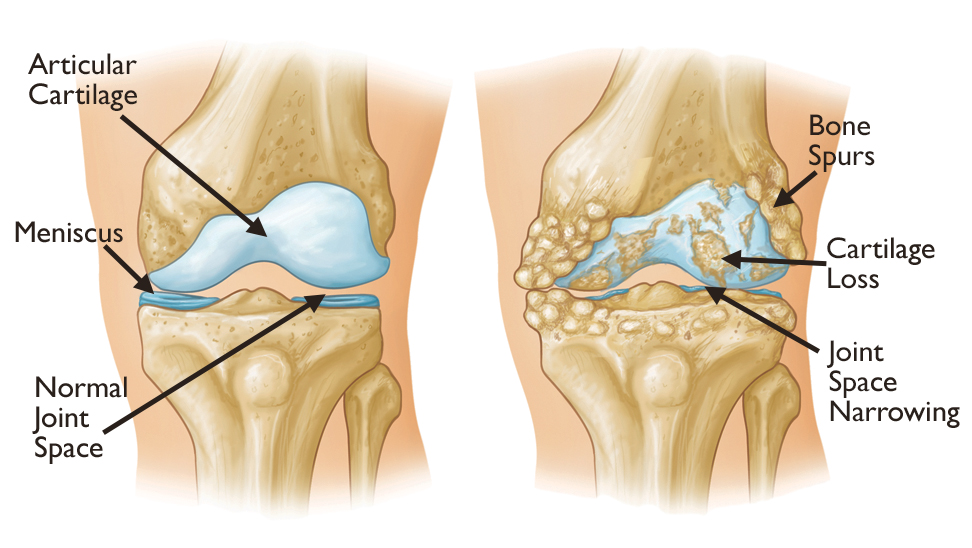
By Fatima Suleiman Halilu and Maryam Bashir Galadanci
Osteoarthritis (O.A), popularly known as a degenerative joint disease (DJD) is commonly defined as the gradual ‘’wear’’ and ‘’tear of the protective tissues at the end of bones that occurs over time with aging. Recent research and clinical evidence have shown that O.A is beyond ‘’ wear’’ and ‘’tear’’ and is an interplay of Physical, biological, and mechanical factors that affects the repair of joint cartilage (protective soft tissue for shock absorption) and surrounding structures leading to changes in joint structures. It is the most common type of arthritis and a major cause of pain in the elderly.
Osteoarthritis affects over 520 million people globally. According to research, there has been a 48% increase in osteoarthritis cases from the year 1990 to the year 2019 and the figures are expected to rise in the coming years. It is a major cause of disability in developing and developed countries and is expected to increase as the population ages. In age groups below 50yrs, men are more often affected, while in the older population the disease is more common in women with a ratio of 2:1 (due to a decrease in sex hormones with menopause). Research on the prevalence of O.A in Africa remains scarce, but a study carried out in South Africa revealed 55.1% of those affected in the urban population and about 87.2% in the rural population are adults aged 65 and above. A certain study on reported cases in healthcare facilities in Nigeria estimated that about 3.3 -7.1% of the population of the country have O.A. This figure is however believed not to be the true value of the cases in the community as there is still little awareness of the condition and more research needs to be carried out.
Osteoarthritis can affect any joint, but the most commonly affected of them are the weight-bearing joints (knee, hip, and spine). With aging over time and repetitive weight bearing on these joints, they start to deteriorate in function. Knee O.A accounts for about 60% of diagnosed O.A cases.
There are two types of O.A: Primary O.A and secondary O.A. The causes of primary O.A are still unclear but genetics is believed to play a role in it. Secondary O.A is caused by s specific triggers that exacerbate cartilage breakdown. Examples of such triggers are joint, injuries, metabolic and inflammatory diseases, Inactivity, and Abnormal mechanical forces.
Signs and symptoms include Pain, stiffness, limitations in movement, a snap/crackle and pop Sound (crepitus) while moving the joints, Muscle weakness, Mild Swelling, tenderness and decreased quality of life. Some joint-specific symptoms might also set in.
Risk factors include Age above 45, Female gender, Overweight or Obesity, Genetics, Trauma or injury to the joints, repetitive stress, sports injuries, joint malalignment, Bone deformities, Occupations that involve certain repetitive movements like bending and prolonged standing, and living a sedentary lifestyle.
Complications that might arise due to O.A include Loss of muscle bulk(atrophy), joint instability, joint deformity, balance impairments and fall risks, neurological symptoms, disability, and depression.
Osteoarthritis is diagnosed through detailed patient history taking, physical examinations, and some special tests. An X-ray may sometimes be done to determine the extent of changes in the affected joint or to eliminate other similar conditions like gout arthritis. CT and MRIs are rarely done. Lab tests might also be carried out if there is a need to rule out conditions like septic arthritis and rheumatoid arthritis.
Osteoarthritis is a chronic, progressive lifelong condition that cannot be cured. Symptoms can, however, be managed conservatively and the disease progression slowed down through the use of medications, supplements, intra-articular injections, diet, lifestyle adjustments, weight loss, and Physiotherapy. In severe cases, joint replacement surgery might be required.
The World Health Organisation recommends Physiotherapy as the first line of management for osteoarthritis. Physiotherapists are specialized health care professionals concerned with improving human function, and movement and maximizing physical potential. On September 8th each year, World Physiotherapy (formerly the World Confederation of Physical Therapy, WCPT) marks World Physiotherapy day as a day to celebrate the profession worldwide and create awareness of health issues concerned with the profession. The 2022 World Physiotherapy theme is ‘’Osteoarthritis and the role of Physiotherapy’’.
Physiotherapists play a vital role in the management of O.A. Their roles span from preventive, to conservative management to pre-and post-joint replacement surgery management. In the preventive stage, Physiotherapists educate patients, clients, and the general public on, the causes, effects, and risk factors of osteoarthritis. Modifiable risk factors like being overweight/ obese and sports injuries can be addressed and managed by a Physiotherapist. Preventive measures are also given.
The conservative role of physiotherapy in osteoarthritis is aimed at slowing down the disease progression, preventing occurrences in other joints, fall prevention, and management of symptoms like pain, swelling, joint stiffness, joint instability, tenderness, impaired mobility, or balance. Physiotherapy also helps improve muscle strength, joint motion, and flexibility, and encourages participation in daily activities with ease. Additionally, Physiotherapists encourage weight loss and design exercises to cater to that. All this ultimately improves the patient’s quality of life. Methods and techniques applied to achieve this include Range of motion exercises, muscle strengthening exercises, stretching exercises, balance exercises, aerobic exercises, functional activity exercises, manual therapy, joint mobilizations, hot and cold therapy, electrotherapy, hydrotherapy (exercises on water) Muscle energy techniques, use of orthotic devices like a knee brace, splint, neck collar, use of a cane and other mobility aids. The type, frequency, and intensity of the exercises, treatment plan, and materials used are dependent not only on the joint structures and muscles affected or the extent of their affectation but also on other factors like the Patient’s goals, age, gender, occupation, body mass index and the presence of other medical conditions. lifestyle. activity level, exercise tolerance, and sometimes beliefs influence management plans. A well-detailed history taking, physical assessment, investigations, and special tests will help your Physiotherapist design a personalized treatment plan that best suits you. These treatment plans are progressive and will usually get improved or adjusted over time with patient improvement or lack of it. Your Physiotherapist will also advise you on a diet, lifestyle adjustments, coping strategies, proper posture, ergonomic/workplace adjustments, and practices.
In cases where conservative management like Physiotherapy fails or certain symptoms and complications set in, Surgery is required. Physiotherapy plays an important pre-and post-operative role in joint replacement surgeries. In the pre-operative phase, patients are assessed holistically and educated on what to expect after surgery including precautions to take and absolute restrictions. They are informed of symptoms to expect like pain, possible swelling, restricted movement, and muscular weakness and how their Physiotherapists can help address them. Their goals are being put into consideration and they are being taught bed exercises and safe transfer methods.
Physiotherapy may commence a few hours after surgery taking into consideration the general health status of the patient and the type of surgical procedure done. A Physiotherapist would perform a detailed assessment and design an appropriate treatment plan according to patient needs, goals, and capabilities. This aims to promote patient independence, address post-surgical symptoms, prevent complications, improve the general health status of the patient and reduce hospital stay. Strengthening exercises, aerobic exercises for improved cardiovascular function, mobility and transfer training, balance and coordination exercises, and walking re-education are among the strategies employed by Physiotherapists post-joint replacement surgeries. Your physiotherapist will be responsible for training you to make use of assistive aids like a wheelchair, walking frames, and canes, graduating you in stages and eventually weaning you off to encourage functional independence. In-patient discharge rules and outpatient appointment sessions for follow-ups, monitoring, and progression are usually given to patients. This has proven to improve the outcome of surgery.
For consultations, and more information about Physiotherapy and Osteoarthritis, contact the nearest Physiotherapist to you. Also, check www.world.physio/wptday and https://nsphysio.org/.
MYTHS VS FACTS:
| MYTH | FACT |
| O.A is a disease of old age | While most cases of O.A are diagnosed from ages 45 and above, younger people do get O.A |
| Exercises and activities worsen O. A | While certain movements, exercises, and activities might worsen O.A symptoms, a carefully planned exercise regimen by a qualified Physiotherapist can help manage the symptoms of O.A and improve quality of life. |
| O.A is caused or triggered by cold weather | There is no evidence that cold weather causes O.A. However, people are more likely to be inactive during cold seasons. This triggers O.A symptoms in an already affected joint |
Fatima Suleiman Halilu PT, and Maryam Bashir Galadanci PT, are members of Kano State Chapter of Nigeria Society of Physiotherapy (NSP)
Related
You may like
Opinion
Dupe and Her Clueless, Asinine Independence Declaration
Published
1 week agoon
April 16, 2024By
Eric
By Sola Ojewusi
In a display marked by both confusion and a deep lack of political insight, Dupe Onitiri-Abiola, took it upon herself last week to lead a splinter group of agitators into declaring an ill-conceived independence for the Yoruba nation.
Broadcasting from her undisclosed location in the United States, Onitiri-Abiola attempted to sever the bonds that have historically united the Yoruba people with the broader Nigerian state. This declaration, dripping with radical fervor and untethered from the realities of international diplomacy and domestic welfare, stands as a stark and embarrassing contrast to the rich political heritage and organizational sagacity of the Yoruba, who are known for their significant contributions to the Nigerian federation and their sophisticated approach to governance. The act not only undermines the notion of sovereignty as understood and respected within the larger framework of nation-states but also appears as a misguided assault on the cultural and political sensibilities of the Yoruba people, amongst whom is the current President of Nigeria—a position that exemplifies the peak of Yoruba involvement in national leadership.
This act of rebellion was not just a misguided venture into political activism; it was a strategic blunder that threatened to alienate Onitiri-Abiola and her miserable followers from the mainstream Yoruba community and the Nigerian state at large. By choosing to broadcast her declaration from the safety of America, Onitiri has demonstrated a troubling detachment from the on-the-ground realities faced by the people in whose name she purports to speak. The clandestine nature of the declaration, shrouded in secrecy and executed from a foreign land, raises questions about the legitimacy and sincerity of her intentions. It also betrays a fundamental misunderstanding of the unity and collective aspirations of the Yoruba people, who, despite various internal disagreements, have largely chosen to pursue their objectives within the democratic and constitutional framework of Nigeria. This rash decision is not only capable of jeopardizing the political stability of the region but has also risked inciting unnecessary conflict, potentially drawing the Yoruba people into a divisive and destructive confrontation with the Nigerian government.
Furthermore, Onitiri’s unilateral declaration could have far-reaching implications beyond the immediate political turmoil. It acts as a dangerous precedent that could inspire similar secessionist movements, undermining national cohesion and destabilizing the delicate ethnic balance that Nigerian leaders have worked hard to maintain. This move, seen as anathema to the principles of unity and collective progress, could isolate the Yoruba community, potentially stripping them of their power to influence national policy and diminish their role in shaping the future of Nigeria. The recklessness of this declaration, therefore, cannot be overstated—it is not only a betrayal of the Yoruba’s storied legacy of diplomacy and political acumen but also a clear and present danger to the stability and unity of the entire Nigerian state. It is imperative for both the Yoruba leadership and the national government to swiftly and decisively address this challenge, reaffirming their commitment to a united Nigeria and discrediting Onitiri’s divisive antics as the political folly they truly represent.
The manifesto, articulated by Onitiri and her cohort, reeks of an asinine understanding of nation-building and the nuanced dynamics of Nigerian federalism. It is a puerile attempt at secession, steeped in anachronistic rhetoric that belongs more to a bygone era of blunt instruments than to our current age of sophisticated governance. This attempt is not only ill-advised but blatantly treasonable, constituting a direct assault on the unity and integrity of the Nigerian state.
It is the height of folly that Onitiri-Abiola, a renegade outlier, would presume to speak for the Yoruba people, whose historical gravitas and intellectual acumen are well-documented and respected across Nigeria and beyond. Her declaration is an affront to the Yoruba’s profound contributions to the fabric of national cohesion and their long-standing investment in the democratic project of Nigeria. This rogue declaration of independence is thus not only unmitigated in its lack of wisdom but also treasonable in its intent. I am sure her purported husband, Chief MKO Abiola would be roiling in his revered grave, regretting the association of his decent name to this obnoxious adventure.
This debacle is further exacerbated by the suspicion that Onitiri-Abiola and her ragtag group of agitators are mere puppets in a larger, more sinister agenda to fragment the unity of the Yoruba race and, by extension, the whole Nigerian federation. The timing of such a declaration, when a son of the Yoruba soil leads the nation, suggests a disturbing endeavor to sow discord and weaken the formidable influence the Yoruba wield in Nigeria’s political sphere.
Indeed, the action by Onitiri’s faction is tantamount to a betrayal of the Yoruba people, an ethnic group known for its sophisticated politicking and strategic acumen. To declare independence in such a frivolous and thoughtless manner is not only a disservice to the Yoruba nation but also an unforgivable insult to the collective intelligence of its people.
In conclusion, the declaration of independence by Dupe Onitiri Abiola and her misguided followers is a quixotic fantasy, a juvenile escapade that flies in the face of political reality and rational thought. It undermines the legitimate aspirations of the Yoruba people and derails the significant progress made in fostering ethnic solidarity and national unity in Nigeria. As such, it should be regarded with the contempt it deserves and dismissed as the clueless, asinine act that it truly is. The Yoruba, and indeed all Nigerians, must stand together against such reckless endangerments to their collective destiny and continue to strive for a harmonious and united Nigeria.
Related
Opinion
Building Leaders Through Character Management in the 21st Century
Published
2 weeks agoon
April 13, 2024By
Eric
By Tolulope A. Adegoke
“Character builds a nation; it builds kingdoms, empires, families, and the world at large. Character tames freedom so as not to abuse absolute power; it promotes sustainable peace and global development, guaranteeing the handing over of a better world to the coming generation.” – Tolulope A. Adegoke, AmbP-UN, PhD., FIMC, CMS, CIV, MNIM
This article, by implication of its contents, aims to solve the societal menace that has ravaged, hampered, and tampered with the spinal cords of the majority of leaders in the Third World Countries, which has its roots in what I refer to as Untamed Freedom- the root cause of Character failure in humans, corporates, and nations at large. We all must understand that true leadership penetrates into the core aspect of human relations and endeavors, which helps to nurture, build, and deliver the authentic requirement for true and sustainable leadership, and how it affects the economy and politics of nations and the world at large. It focuses on ‘Character’ as the main and authentic key for leadership, how relevant it could be and why and as well how to harness it to building future leaders locally, nationally, and globally for the benefits of mankind. It also delved into the internal affairs of some developing nations in the world and how they have suffered from ineffective leadership practices through unethical conduct. It also looked into how ‘Ethics’ could be said to be a disturbing aspect of leadership and how it has so much affected the majority of the Third World Countries who are having issues in handling sustainable leadership. It therefore concludes with how a nation like Nigeria could enlarge its coasts by judiciously maximizing its endowments through effective ‘Character’ in individual and joint leadership endeavors, thereby enlightening the readers with the facts that character sees people as great ASSETS and not properties. The researcher adopted Historical and Thematic Analysis in carrying out the research.
I ponder so hard on ‘How do we then build leaders of today? I shall focus on the Power of Character (as vital requirement for leadership in Nation Building)’ with the aim of building capacity through greater enlightenment strategy towards fixing today, and as well handing over a better world to coming generations globally. Do you know why leaders are so weak in many developing countries of the world? The reason is that they lack CHARACTER. Lack of character is what makes bad leadership, and bad leadership is what breeds gross mismanagement and misconducts, while misconducts and mismanagement are what destroy or impede national growth and development. Bad leaders are one thing in the day and another thing at night! They make deals that are shady and then look pretty or handsome on the camera. They rule instead of leading; they grind instead of guiding. The Book of Life (Bible) says, God is the same Yesterday, Today, and Forever! It also reveals that Night and Day are the same to God! This is a clear indication that God has CHARACTER! And He has given unto us the same thing called CHARACTER! If you are going to be what you were born or created or desired to be (future leaders), then, you must develop the first principle God gave to us (MAN) which is CHARACTER! For us to deliver the present and future, and as well fulfill divine intentions (purpose), we need to study God Himself and His manner of operations and creations according to Genesis chapter 1 verses 26 (NKJV): ‘Let us make Man in Our IMAGE after our likeness: and let them have DOMINION over the fish of the sea, and over the fowl of the air, and over the cattle, and over all the earth, and over every creeping thing that creepeth upon the earth.’ Nothing is therefore IMPOSSIBLE, because I and you came out of God. He is the most authentic leadership example to be followed; He has made us in His IMAGE and LIKENESS to have DOMINION over the works of His Hands. It should be noted that the first gift given to Man by God is IMAGE. Whatever God gives you first is what you need first.
What is IMAGE? Image simply means CHARACTER. God said let Man have my CHARACTER. The most important thing you need to become what you were born to be (which is a LEADER) is CHARACTER. The number one fitness in leaders today is CHARACTER. It is the foundation of leadership! Everybody was born to be a leader, but, we are not meant to rule over people! Leaders lead by examples, guides by principles, and guard by strategies. Leaders lead in specific areas of gifting or expertise. The word CHARACTER means FIXED, PREDICTABLE, STATUE, SET, STABLE, STEADY, DEPENDABLE, READY, and WORK! These are qualities which are unchanging and dependable like the STATUE. For example, have a good look at a STATUE; what is it doing where you put it or fix it? Whatever inflictive words you say to the ‘statue’, it still stands? That is simply CHARACTER! As a leader that you are wired or desired to be, can we trust you to be the same, even in the dark? Are you the same person when no one is watching? What would you do if none would ever find out? What are those things you secretly do on your mobile phones or laptops or on the internet? Are you the same person all the time? Are you the same person even when given freedom or power? When life rains on you, are you the same person? Are you the same person, no matter what people say to you or about you? That is why Third World Countries are having issues handling true and sustainable leadership! What is commonly present in those regions of the world are RULERS not LEADERS, due to lack of CHARACTER.
Requirements of Character for Sustainable Leadership Do you have CHARACTER? When you change location, are you still the same person? LEADERSHIP demands CHARACTER. A reliable example of Character is PRINCIPLE, because it is Constant, it never changes. When you throw something up, it falls down… it is like that everywhere. Leadership requires CONSISTENCY! This is because the will of God never changes. No matter where you go, gravity is constant. Do you have Character? I want you to keep encouraging yourself to keep on developing CHARACTER. As future leaders, who are empowered to save the future, to impacts our world positively, we must be unchanging (i.e consistent on the positive sides) if truly we are going to develop our powerful leadership capacities.
The Disturbing Aspect of Leadership The major disturbing aspect of leadership which most leaders do not consider to develop is ETHICS. Ethics is as a result of character! The power of unethical behavior affects everyone in the community, society, state, nation, and the world at large. Ethics is personal, but it is never private! A few business or political leaders have no ETHICS; they make some unethical moves that can affect everyone. When you violate character, it is a personal decision, but it is not a private issue. You affect all of us. That is why corruption must never be tolerated anytime, because one corrupt person affects everyone. Many developing nations are still struggling with their economy today because of unethical behaviors by a majority which has fully established CORRUPTION as a practice that can now be overlooked, which have crippled the economy of these nations. Many people consider Nigeria a poor nation in spite of all the natural resources she is endowed with (Precious stones, crude oil, very fertile soil among others), because just a few set of people are unethical which affects the entire population in the country. So many investors are currently scared to invest in some part of the developing nations, because there are just a few set of people who would abuse such an investment which has therefore deprived so many people of the opportunities to be employed or t become job owners, just because a few people are unethical. You need to tell your neighbor ‘Do right for my sake’. If great leaders who have been absorbed by history had decided not to do what is right, what do you think would have happened to us today? A few chose to stand right, do right and make right. One decision could have affected the entire world. This is why it is so important for you to have character for the sake of the millions who will look up to you some day! This is why your gift is critical to your generation, but protecting it is much more important. GREED is a matter of CHARACTER. When a research on the major cause of crisis in the world was made, it was said that some set of people had GREED, and greed became a global phenomenon. Discipline powers character for effective leadership. Character and Ethics are national and global security issues. Living right is a global security issue. When you live right, you are simply affecting a lot of people vice-versa.
The Tests and Trials of Leadership Character is developed by ‘testing and trials’. Testing is the development of ETHICS. Character is built or developed through pressure, temptation (trials), and resolve. The credibility of leadership is character! The force of leadership is character! The trust of leadership is character! The legitimacy of leadership is character! The integrity of leadership is character! The reason why people still celebrate Nelson Mandela, Koffi Annan among others is because he was tested and trusted. The reason why Nelson Mandela had so much credibility all over the world is because, while he was alive he went through a test of 25 years in prison, because of a conviction he had, he was just like a statue with this notion: I cannot bend; I am going to jail just like this; I believe in what I see, I believe in a dream, I believe in my convictions, because they are right, I will not compromise, I will not change! Nelson Mandela stayed faithful, he went through the test and trials, and people trusted him. In prison, he was the same, he was beaten mercilessly, he was the same, when he had to cut the rocks with chisel, he was the same, and when he came out of prison he was still the same, and was made the President of South Africa, because he was the same. People could trust him. Even the Dr. Myles Monroe (of blessed memory) once said: ‘People often look at me as if I was born the way I look, but I have been through a lot of things, pressures, scars on my back, tribulations, criticisms, attacks, but I decided, I believe what I believe! I stay steady! The world reads my books, I have been invited to over a hundred and fifty-two nations across the world and they wondered: who is this young man, but I have developed my character through tough times.’ Anybody could begin something, a few people finish! How many things have you begun, how many things have you started managing, how many of it have you finished? Where is your character? Are you steady under pressure? Can you be faithful under being disappointed? Can you still believe when no one is with you? When you have character, you are ready to go alone! Everybody is evil, not me! Everybody is corrupt, not me! Everybody is failing, not me! You have to work by yourself to develop character! Your innate gifts are at the mercy of your character! Your character is more important than your gifts, because without character, you can lose your gifts. That is why God gave Man CHARACTER (His IMAGE) before He gave him DOMINION (Control). Most people lose their provisions because they lost their character! That is why it is important for you to protect yourself by your character (IMAGE), and that is why character (IMAGE) is God’s utmost priority! Character is necessary for DOMINION (Control); it guarantees a tamed-freedom. Character breeds decent followers; then, it builds them into enviable leaders that can ‘MANage’ the natural resources as given them by God, and then, put them into appropriate and decent usage for the good of all mankind. Leadership is simply service to humanity, it is not selfishness, not greed, not abusive…Only character determines and promotes service. Service is followership, help; it is the authentic exhibition of our innate being. Character builds a nation; it builds kingdoms, Empires, family and the world at large. Character tames freedom so as not to abuse absolute power; it promotes sustainable peace and global development that guarantees the handing over of a better world to coming generation. It is a baton which must be passed on and on forever. Life is a mysterious gift given to man by God Almighty embedded with so many hidden treasures… its usage is up to man, but only the deeds of men pollutes it! Character therefore, should not be mistaken for REPUTATION. Reputation has become much more important in the world today than character, and that is a tragedy, because, position has become more important than disposition. As a matter of fact, we need leaders with character, not leaders with personality! Some people have well packaged personality but lack character, yet they are the most celebrated in our world today. Many people are well branded as dignified figures vying for leadership positions, unfortunately, ignorant people rush up to them, vote them in, then the economy and political structure of their countries crashes! Instead of voting the man with CHARACTER (i.e the right IMAGE), which complements leadership to the position of reliable leadership. This is simply the reason why I chose this topic: ‘HOW DO WE BUILD FUTURE LEADERS?’ Which focuses on CHARACTER in Nation Building in today’s world). Nigeria and other developing nations must first of all confront their domestic problems by consolidating their democracy. Democracy is not just the question of holding periodic elections, Important as this is, it means developing a democratic culture underpinned by the rule of law. We must build an egalitarian society with careers opened to talents. It should be possible for any (Nigerian) talent(s) to rise to any position that these talents entitle him or her. We must face the question of the economy squarely. Sixty-three years after independence, we still operate a dependent economy based on export of raw materials and industries of import substitution. We must reverse the process by building industries, particularly agro-based industries in which we have comparative advantage. Nigeria (My Country) can support huge textile and garment industries based on local production of cotton. This is also an industry which the current regime of the World Trade Organization favors for developing countries. The so-called Tiger economies of South East Asia, China and India virtually dominate the textile and garments industry of the world. We ought to be able to compete with Israel and the United States in providing the world with properly packaged tropical fruits. We should cut our tastes for unnecessary luxury goods and use what we can produce. We need to open our market to investments from the outside world. One hopes present policies in this regard would be determinedly pursued. The economy is a major factor to earning respect in the international system and we must do everything to develop our economy. There is no strategy of economic development better than those that have been tried and that have worked in the Western liberal democracies. Any attempt to graft economic development on an authoritarian regime will fail. Character is key factor!
We need to take a look at the example of Botswana (few years ago), when and where honest and liberal government and proper management of national resources and patrimony have led to development. Character sees people as greatest ASSETS and not properties. Value your fellow man greatly, they are the only tool that can stand by your side anytime any day, they shall be the one to continue your leadership processes in the future for the benefits of all as a result of your tremendous impacts on them. The assignment of leaders is not to raise followers, but leaders through greater impacts by living a life of great examples and never to forget to help them with emotional intelligence which is a key factor for leadership inputs and outputs.
Dr. Tolulope A. Adegoke is a Distinguished Ambassador For World Peace (AMBP-UN), and an accredited Effective Leadership Management Trainer. He is also a recognized Fellow, of the Institute of Management Consultants (FIMC), and a Certified Management Specialist (CMS), London Graduate School (LGS).
Related

By Richard Akinnola
Impetuous, garrulous, flippant, compulsively and deliriously narcissistic, that succinctly encapsulates the Nyesom Wike persona. A study of the political trajectory of the FCT Minister shows that he is only loyal to himself and nobody else, irrespective of his feigned allegiance. He may kowtow and genuflect before a political leader, as he is currently doing in Abuja but once he can no longer use you, he goes into a fit of incoherent vituperative verbal assault, denigrating his benefactors.
I watched his recent drama on Channels where he was reeling out his achievements as Governor, he said he built a Cancer Centre and named it after “one man”. He also built a Judicial institute and named it after “one woman”. (Pejoratively referring to Dr Peter Odili and his wife, Justice Mary Odili). His former political leader who he had praised to high heavens is now “one man”. How come his long time political associates suddenly turn enemies? -Rotimi Amaechi, Abiye Sekibo, Celestine Omehia, Austin Opara, Lee Meeba, and now, Dr Peter Odili, among others.
Almost everything that Wike had said in public have been repudiated by him. From the PDP primaries where he vowed to support whosoever emerged as candidate, to his vow not to be minister, to his scathing excoriation of the APC which he likened to a cancerous party, everything Wike supposedly stood for have been repudiated by his fickle mindedness.
Now, he is dancing around PBAT, like an urchin singing nursery rhyme, in his guttural and hoarse voice: “President Tinubu, on your mandate l shall stand”. President Tinubu, Wike is not standing on any mandate. He is standing on his opportunistic position as a minister. Remove him as minister and see if he would still be standing on your mandate. Tomorrow, before the cock crows at night, he would deny you if he is removed as minister and would start lamenting how he supposedly helped you but was used and discarded.
Here was a man who publicly said that Odili saved his political career as Chairman of Obio Akpor local government, leading to his rise in political ascendancy and he used every opportunity to praise and honour Odili and his wife. He followed this up with a public declaration where he was almost swearing thus: “I don’t know the day l would die but l know l would die one day but the truth must be told, any day that l would make Dr Odili and his family cry, may God allow me to go…I would never be alive to make you cry. I will never abandon you and your wife. Where would l have been but for you and your wife? Who am l? From where? My wife would not have been a Magistrate, talk less a Judge but for Mrs Odili. Nobody in this country can make me abandon you and your family. Never. …My wife and l are forever grateful to you for the roles you played in my life”.
This was shown live on CHANNELS. Today, what is Wike doing to the same Odili? Publicly dissing and ridiculing him on same CHANNELS just because Dr Odili refused to queue behind him to decapitate Governor Sim Fubara. As an elder statesman, Odili rather preferred to settle the differences between the duo, which Wike refused. That is Odili’s sin to attract Wike’s “Fatwa”.
He would do same thing to President Tinubu tomorrow if the president does not align with his interest. He doesn’t even understand the dynamics of larger politics to the fact that Odili and PBAT have a long-standing relationship being in the same class of 1999 Governors and that Odili doesn’t even have issues with PBAT. You cannot praise a man to high heavens for eight years in your fit of sycophancy, only to start publicly disrobing him just because he refused to be led by the nose in your ill-conceived political fight with your successor. What that means is that tomorrow, he’ll do same thing to president Tinubu if he doesn’t do his political bidding in Rivers state. That would amount to political self-immolation.
So, if everyone who has assisted you in your political ascendancy are bad, then, something definitely must be wrong with you.
Despite his accomplishments as Governor in terms of project execution which l acknowledge, there is no doubt, Wike has a serious character flaw that only him can cure. But trust me, despite his wealth and “power”, it’s a matter of time, this young man is on his way to political perdition. I pray he doesn’t end that way. Minister Wike, you are an achiever in terms of performance but l pray God grants you wisdom on how to navigate and relate with people who differ from you politically.
Richard Akinnola, a lawyer, activist and public affairs analyst writes from Lagos
Related

How Yahaya Bello Used Kogi’s $720k to Pay Children’s School Fees in Advance – EFCC Chairman

I’ll Resign If Yaya Bello Eacapes Prosecution, EFCC Chair Vows

Nigeria Air Scam: EFCC Arrests Former Aviation Minister, Hadi Sirika

Dana Air Confirms Runway Excursion Involving It’s Aircraft, Says Passengers, Crew Safe

Kwibuka 30: Nigerian Community In Rwanda Visits Kigali Genocide Memorial

FG Mulls Review of Admission Age into Nigerian Universities

Lagos-Calabar Coastal Highway: Prioritize Existing Unfinished Projects, Peter Obi Tells FG

Nigerian Engineer Wins $500m Contract to Build Monorail Network in Iraq

WORLD EXCLUSIVE: Will Senate President, Bukola Saraki, Join Presidential Race?

World Exclusive: How Cabal, Corruption Stalled Mambilla Hydropower Project …The Abba Kyari, Fashola and Malami Connection Plus FG May Lose $2bn

Rehabilitation Comment: Sanwo-Olu’s Support Group Replies Ambode (Video)

Pendulum: Can Atiku Abubakar Defeat Muhammadu Buhari in 2019?

Fashanu, Dolapo Awosika and Prophet Controversy: The Complete Story

Pendulum: An Evening with Two Presidential Aspirants in Abuja

Who are the early favorites to win the NFL rushing title?

Boxing continues to knock itself out with bewildering, incorrect decisions

Steph Curry finally got the contract he deserves from the Warriors

Phillies’ Aaron Altherr makes mind-boggling barehanded play

The tremendous importance of owning a perfect piece of clothing
Trending
-

 News6 years ago
News6 years agoNigerian Engineer Wins $500m Contract to Build Monorail Network in Iraq
-

 Featured6 years ago
Featured6 years agoWORLD EXCLUSIVE: Will Senate President, Bukola Saraki, Join Presidential Race?
-

 Boss Picks6 years ago
Boss Picks6 years agoWorld Exclusive: How Cabal, Corruption Stalled Mambilla Hydropower Project …The Abba Kyari, Fashola and Malami Connection Plus FG May Lose $2bn
-

 Headline6 years ago
Headline6 years agoRehabilitation Comment: Sanwo-Olu’s Support Group Replies Ambode (Video)
-

 Headline6 years ago
Headline6 years agoPendulum: Can Atiku Abubakar Defeat Muhammadu Buhari in 2019?
-

 Headline5 years ago
Headline5 years agoFashanu, Dolapo Awosika and Prophet Controversy: The Complete Story
-

 Headline6 years ago
Headline6 years agoPendulum: An Evening with Two Presidential Aspirants in Abuja
-

 Headline6 years ago
Headline6 years ago2019: Parties’ Presidential Candidates Emerge (View Full List)

